Applications
The Injectrode has been successfully placed on more than 20 nerves in preclinical and human cadaver models.
The images and videos below show the Injectrode discreetly placed entirely beneath the skin, practically invisible on the outside. That means no protruding wires or a bulging IPG. Once on the nerve target and stimulation is desired, the Injectrode is externally stimulated by an external pulse generator (EPG), keeping all electronics out of the body. Future users don't need to wear anything when not stimulating.
Read below to learn why the Injectrode may be very suitable for each nerve target.
Chronic Pain
(click the nerve target for more info)
Post-Op & Post-Traumatic Pain
Bladder, Bowel, & Sexual Dysfunction
Hypertension & Heart Failure
Epilepsy
Post-Stroke Recovery
Obstructive Sleep Apnea
Inflammation
Cluster Headaches & Migraines
Suprascapular/
Axillary Nerves
Branching from the brachial plexus, the axillary and suprascapular nerves have been treated with peripheral nerve stimulation in response to shoulder injuries and subacromial impingement syndrome, and arthritis. The suprascapular nerve is primarily targeted, and the axillary as a secondary target as needed.
Mansfield JT, Desai MJ. Axillary Peripheral Nerve Stimulation for Chronic Shoulder Pain: A Retrospective Case Series. Neuromodulation. 2020 Aug;23(6):812-818. doi: 10.1111/ner.13096. Epub 2020 Jan 13. https://www.neuromodulationjournal.org/article/S1094-7159(21)00242-7/fulltext
Lumbar Dorsal Rami
The lumbar dorsal rami are associated with lower back pain, a herniated disc, facet joint syndrome, and weakness of one or more lower back muscle groups. Chronic medial branch pain has been successfully treated with peripheral nerve stimulation.
Tieppo Francio V, Westerhaus BD, Rupp A, Sayed D. Non-Spinal Neuromodulation of the Lumbar Medial Branch Nerve for Chronic Axial Low Back Pain: A Narrative Review. Front Pain Res (Lausanne). 2022 Feb 25;3:835519. https://doi.org/10.3389/fpain.2022.835519
Dorsal Root Ganglia & near Dorsal Root Ganglia
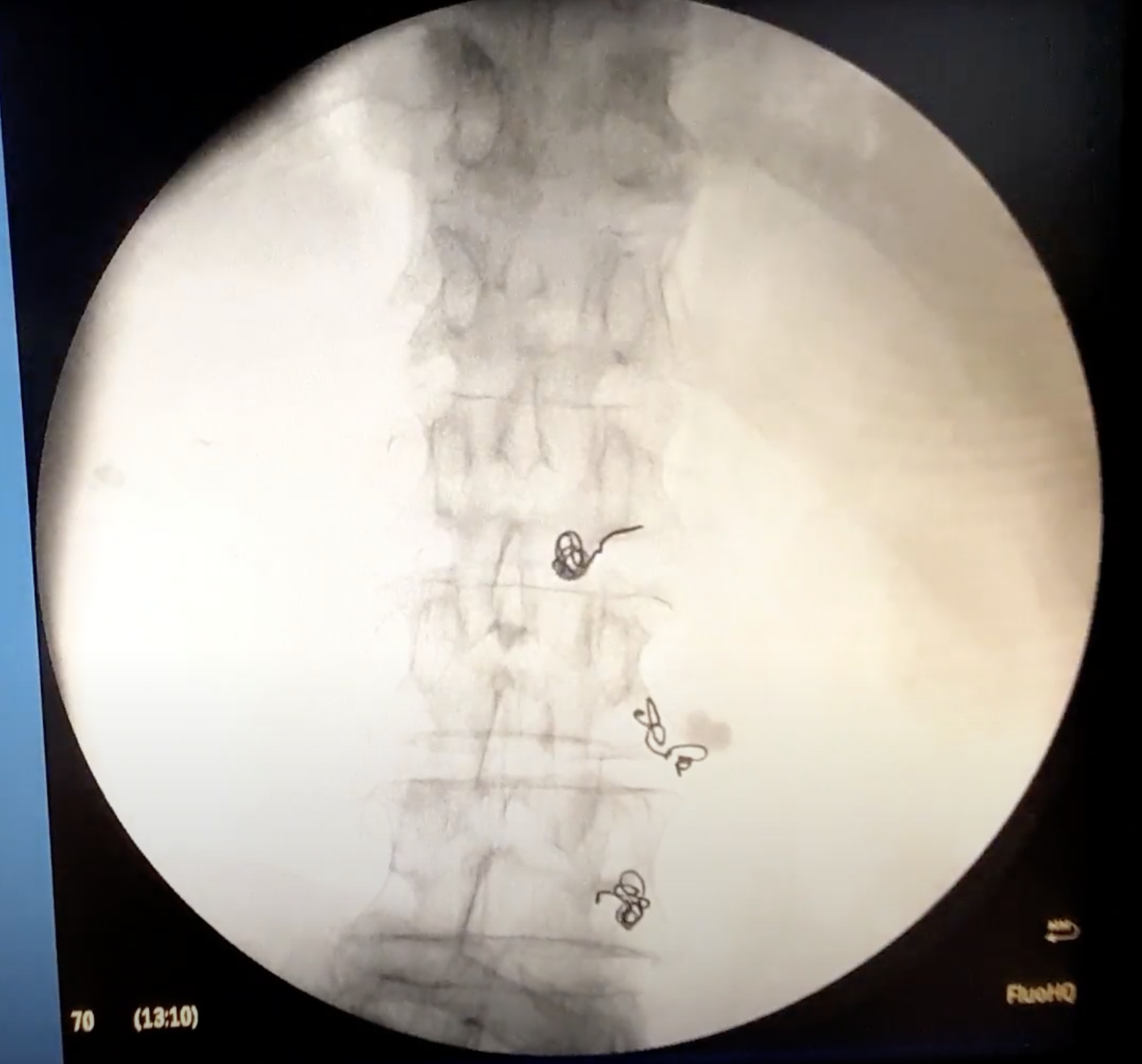
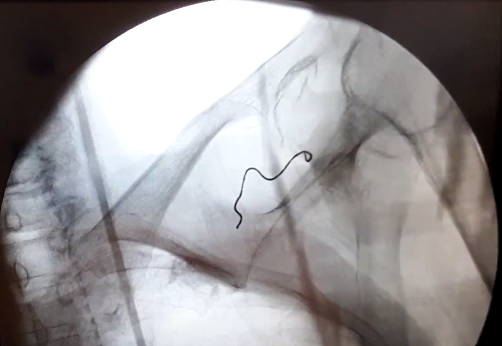
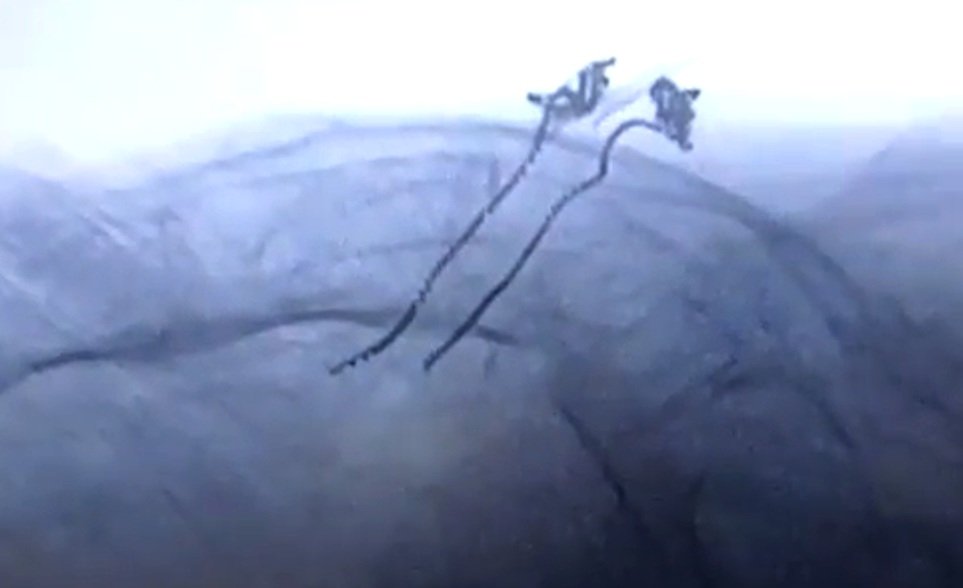
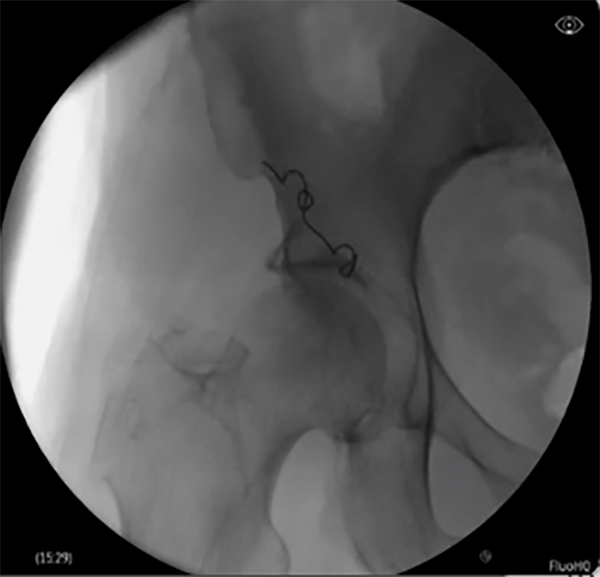
Neuromodulation devices targeting the dorsal root ganglion and nerves as well as nerve rootlets connecting into the DRG have technically challenging and time-consuming placement procedures. The Injectrode’s innovative placement procedure, with only 5 steps, has simplified how leads near the DRG can be placed. Relying on a transforaminal approach, similar to steroid injection pathways, present a development of a promising, minimally invasive alternative to the current standard of care.
The ‘scotty-dog’ landmark allows for repeatable injection of the device stimulator on the dorsal aspect of the roots as they exit the foramen. The delivery needle may be positioned between the likely location of the DRG and the pedicle at an oblique angle, then advanced off the bone to enter the dorsal aspect of the foramen. In this placement approach, the epidural space is not entered, and the Injectrode’s position relative to the ganglion enables stimulation.
Large animal and cadaver studies are underway to further characterize this placement approach.
Sacral Roots
Sacral root stimulation has been shown to improve urinary, bowel, and sexual dysfunction.
Research is underway to assess the potential use of Injectrode powered sacral stimulation for the treatment of Inflammatory Bowel Disease (IBD, Crohn's disease, and ulcerative colitis) and other inflammation-related conditions.
de Oliveira PS, Reis JP, de Oliveira TR, Martinho D, E Silva RP, Marcelino J, Gaspar S, Martins F, Lopes T. The Impact of Sacral Neuromodulation on Sexual Dysfunction. Curr Urol. 2019 Jul;12(4):188-194. doi: 10.1159/000499307. Epub 2019 Jul 20. PMID: 31602184; PMCID: PMC6738141.
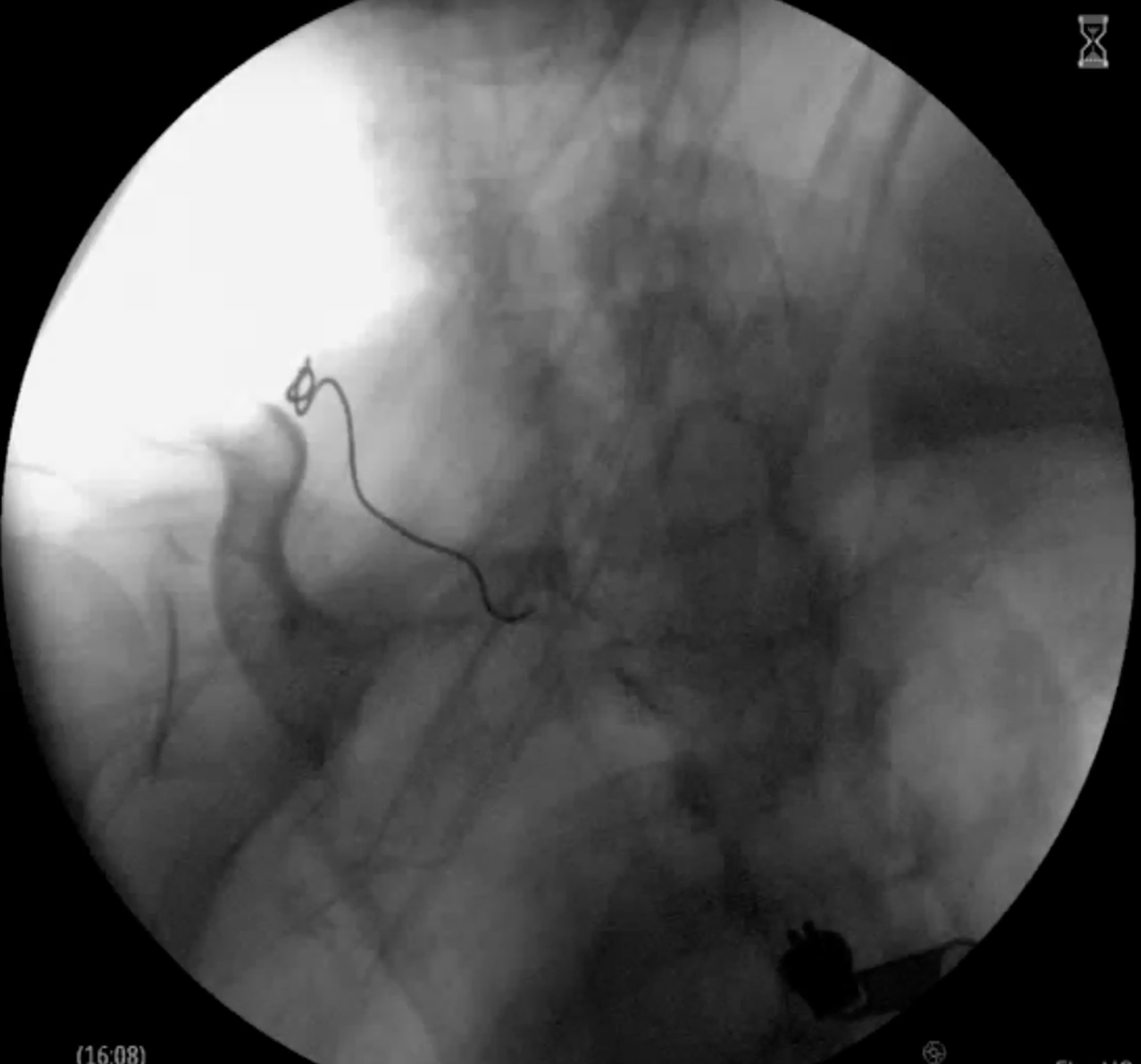
The sphenopalatine ganglion (SPG) is a well-known target for injected anesthetics, steroids, and ablation to treat cluster headaches, trigeminal neuralgia, and craniofacial pain. This target is particularly challenging, as the location is highly mobile and patients have difficulty limiting movements of implanted electronics.
An Injectrode placement procedure for the SPG was devised to maximize patient comfort for transcutaneous stimulations.
We developed a procedure in which the delivery needle was inserted inferior to the zygomatic arch and anterior to the mandible. Then, the needle was advanced toward the pterygopalatine fossa until contact was made with the lateral pterygoid plate. The point of entry under the earlobe allows patients to apply stimulation readily through a surface patch.
Movement of the head in flexion and extension, lateral rotation, and opening and closing of the mouth for repeated cycles led to negligible movement of the stimulator and collector ends.
This approach is a promising first step in demonstrating how the Injectrode can be used to treat craniofacial pain.
Sphenopalatine Ganglion
Saphenous/
Genicular Nerve
Chronic pain attributed to the knee joint, including the genicular and saphenous nerves, may be associated with knee trauma and osteoarthritis. Persistent pain post-TKA is often treated with Genicular PNS.
Chitneni A, Berger AA, Orhurhu V, Kaye AD, Hasoon J. Peripheral Nerve Stimulation of the Saphenous and Superior Lateral Genicular Nerves for Chronic Pain After Knee Surgery. Orthopedic Reviews. 2021;13(2). doi:10.52965/001c.24435 https://orthopedicreviews.openmedicalpublishing.org/article/24435-peripheral-nerve-stimulation-of-the-saphenous-and-superior-lateral-genicular-nerves-for-chronic-pain-after-knee-surgery
Posterior Tibial Nerve
Another common neuromodulation target is the posterior tibial nerve (PTN). The Injectrode’s placement procedure allows clinicians to customize the size of each anchor (stimulating anchor, central anchor, subcutaneous collector) for each patient’s unique anatomy.
Out of plane ultrasound imaging can be used to easily identify the target nerve and allow for needle trajectory planning to minimize tissue trauma. The delivery needle is guided to the target and is angled roughly parallel to the nerve for Injectrode deployment. The Injectrode’s flexibility makes the PTN a suitable target, as the device conforms to the PTN, with the stimulating anchor capable of curving around the nerve after placement.
By creating a low-resistance path, the Injectrode is a promising approach for the future of PNS treatment.
Sciatic Nerve
Chronic sciatic pain may be associated with degenerative disc disease and intervertebral disc hernation, and diabetes, among other conditions.
Femoral Nerve
Femoral nerve pain has been associated with postoperative ACL reconstruction pain.
Busch C, Smith O, Weaver T, Vallabh J, Abd-Elsayed A. Peripheral Nerve Stimulation for Lower Extremity Pain. Biomedicines. 2022; 10(7):1666. https://doi.org/10.3390/biomedicines10071666
Greater Occipital Nerve
Occipital nerve stimulation may be a promising treatment modality for patients with chronic headache who present with features of occipital neuralgia.
Salmasi V, Olatoye O, Suolieman Terkawi A, Hah J, Ottestad E, Pingree M. Peripheral Nerve Stimulation for Occipital Neuralgia. Pain Medicine. 21(1), S13-S17 (2020). https://doi.org/10.1093/pm/pnaa083
Intercostal Nerves
Intercostal neuralgia may arise from rib fractures, herpes zoter, and chronic abdominal pain.
Johnson RD, Green AL, Aziz TZ. Implantation of an intercostal nerve stimulator for chronic abdominal pain. Ann R Coll Surg Engl. 2010 Apr;92(3):W1-3. doi: 10.1308/147870810X12659688851474. https://pubmed.ncbi.nlm.nih.gov/20412657/
Ulnar/Median/
Radial Nerves
The ulnar, median, and radial nerves associated with cubital tunnel, carpal tunnel, and radial tunnel, respectively, in addition to CRPS, have been successfully treated with peripheral nerve stimulation PNS.
Jeon IC, Kim MS, Kim SH. Median Nerve Stimulation in a Patient with Complex Regional Pain Syndrome Type II. J Korean Neurosurg Soc. 2009 Sep;46(3):273-6. doi: 10.3340/jkns.2009.46.3.273. Epub 2009 Sep 30. PMID: 19844632; PMCID: PMC2764030.
Pudendal Nerve
Lam CM, Keim SA, Latif UNovel implantation technique for pudendal nerve peripheral nerve stimulation for treatment of chronic pelvic painRegional Anesthesia & Pain Medicine Published Online First: 06 July 2023. doi: 10.1136/rapm-2023-104551
Chronic pelvic pain due to irritable bowel syndrome and endometrosis is associated with the pudendal nerve.
Obturator Nerve
Tipton JS. Obturator neuropathy. Curr Rev Musculoskelet Med. 2008 Dec;1(3-4):234-7. doi: 10.1007/s12178-008-9030-7. Epub 2008 Jun 11. 10.1007/s12178-008-9030-7
Chronic pain originating at the obturator nerve is commonly found in athletes due to fascial entrapment.
Brachial Plexus
Postoperative brachial plexus pain after a rotator cuff repair procedure has been treated with peripheral nerve stimulators.
Ilfeld B, Plunkett A, Vijjeswarapu A, Hackworth R, Dhanjal S, Turan A, Cohen S, Eisenach J, Griffith S, Hanling S, Sessler D, Mascha E, Han Y, Boggs J, Wongsarnpigoon A, Gelfand H. Percutaneous Neuromodulation of the Brachial Plexus and Sciatic Nerve for the Treatment of Acute Pain Following Surgery: Secondary Outcomes From a Multicenter, Randomized, Controlled Pilot Study. Neuromodulation: Technology at the Neural Interface. 2023; 26(3): 638-649. https://doi.org/10.1111/ner.13492.
Carotid Sinus Nerve
The carotid sinus nerve, innervating the baroreceptors of the carotid artery, has been targeted with stimulation to treat angina pectoris, heart failure, and resistant hypertension.
Cracchiolo M, Ottaviani MM, Panarese A, Strauss I, Vallone F, Mazzoni A, Micera S. Bioelectronic medicine for the autonomic nervous system: clinical applications and perspectives. J. Neural Eng. 2021;18(4). 10.1088/1741-2552/abe6b9.
Vagus Nerve
Vagus nerve stimulation (VNS) has been shown to improve quality of life in individuals with heart failure, post-stroke recovery, rheumatoid arthritis, and other inflammatory conditions.
An implantable vagus nerve stimulator has been approved by the FDA to treat epilepsy and depression. VNS may prevent or lessen seizures by sending regular, mild pulses of electrical energy to the brain via the vagus nerve.
Another vagus nerve stimulation device is FDA-approved to be used with rehabilitation when recovering from a stroke.
Asad Z, Stavrakis S. Vagus nerve stimulation for the treatment of heart failure. Bioelectronics in Medicine 2019 2:1, 43-54. https://doi.org/10.2217/bem-2019-0012.
https://www.mayoclinic.org/tests-procedures/vagus-nerve-stimulation/about/pac-20384565
https://www.epilepsy.com/treatment/devices/vagus-nerve-stimulation-therapy
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00475-X/fulltext
Trigeminal Nerve
The trigeminal nerve has been targeted to treat drug-resistant epilepsy.
Gil-Lopez F, Boget T, Manzanares I, Donaire A, Conde-Blanco E, Bailles E, Pintor L, Setoain X, Bargallo N, Navarro J, Casanova J, Valls J, Roldan P, Rumia J, Casanovas G, Domenech G, Torres F, Carreno M. External trigeminal nerve stimulation for drug resistant epilepsy: A randomized controlled trial. Brain Stimulation. 2020; 13(5). 1245-1253. https://doi.org/10.1016/j.brs.2020.06.005.
Hypoglossal Nerve
Electrical stimulation of the hypoglossal nerve can help with obstructive sleep apnea (OSA). Access to the nerve in the neck without the need for surgery may provide a tectonic shift in the field.
Olson M, Junna M. Hypoglossal Nerve Stimulation Therapy for the Treatment of Obstructive Sleep Apnea. Neurotherapeutics. (2021) 18, 91-99. https://doi.org/10.1007/s13311-021-01012-x.